Skip to main content
Browse Issues
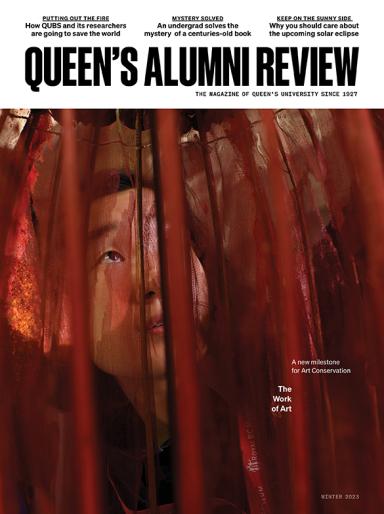
2023
2022
2021
2020
2019
Fall 2019

Summer 2019
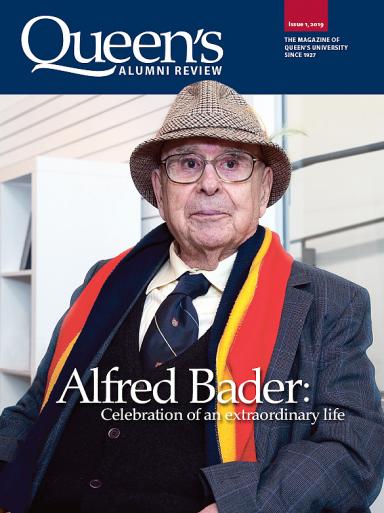
Spring 2019
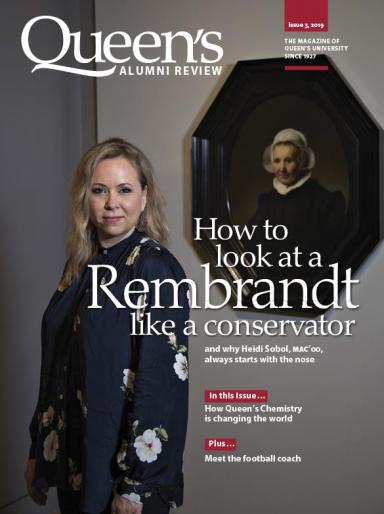
Winter 2019
2018
Fall 2018
Summer 2018
Spring 2018
Winter 2018

2017
Fall 2017
Summer 2017
Spring 2017

Winter 2017
2016
Fall 2016
Summer 2016
Spring 2016
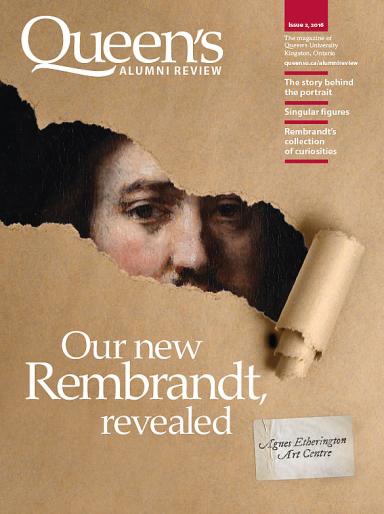
Winter 2016
2015
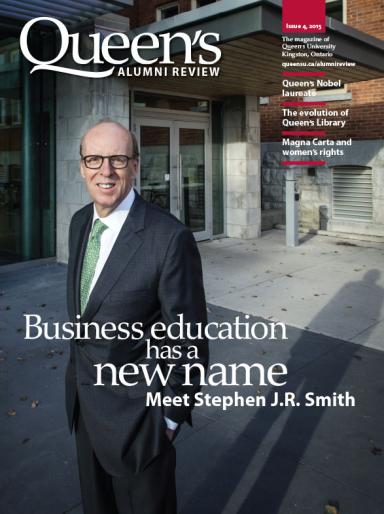
Fall 2015
Summer 2015

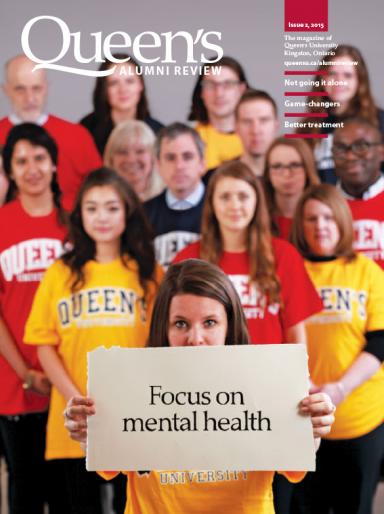
Spring 2015
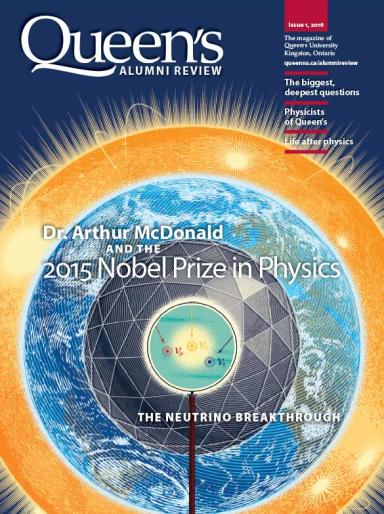
Winter 2015
2014
Fall 2014
Summer 2014
Spring 2014
Winter 2014

2013
Fall 2013

Summer 2013

Spring 2013

Winter 2013

2012
Fall 2012
Summer 2012

Spring 2012
Winter 2012

2011
Fall 2011

Summer 2011
Spring 2011

Winter 2011
2010
Fall 2010
Summer 2010

Spring 2010
Winter 2010
2009
Fall 2009

Summer 2009
Spring 2009