Research in the Stroman Lab has two main branches; 1) identify how pain processing is altered in fibromyalgia (FM), and 2) development of fMRI methods for pain research. This research has been progressing for over 25 years.
 Pain isn’t just a sensation, it’s our cognitive and emotional response too, and it serves an important purpose. When pain processes aren’t working properly, this can result in chronic pain, or can cause of to feel pain from stimuli that shouldn’t normally be painful (like touch). We need to understand how this pain processing system works in humans in order to understand how (and detect when and where) it is going wrong in chronic pain conditions such as Fibromyalgia.
Pain isn’t just a sensation, it’s our cognitive and emotional response too, and it serves an important purpose. When pain processes aren’t working properly, this can result in chronic pain, or can cause of to feel pain from stimuli that shouldn’t normally be painful (like touch). We need to understand how this pain processing system works in humans in order to understand how (and detect when and where) it is going wrong in chronic pain conditions such as Fibromyalgia.
Pain serves the vital purpose of motivating us to reduce or avoid injury, and to protect injuries while they heal. How we feel pain can change depending on if we are sick, injured, or upset. We can learn what causes pain and how to anticipate it, and we can form expectations on how it will feel. All of these factors change how we experience pain at any given circumstance.
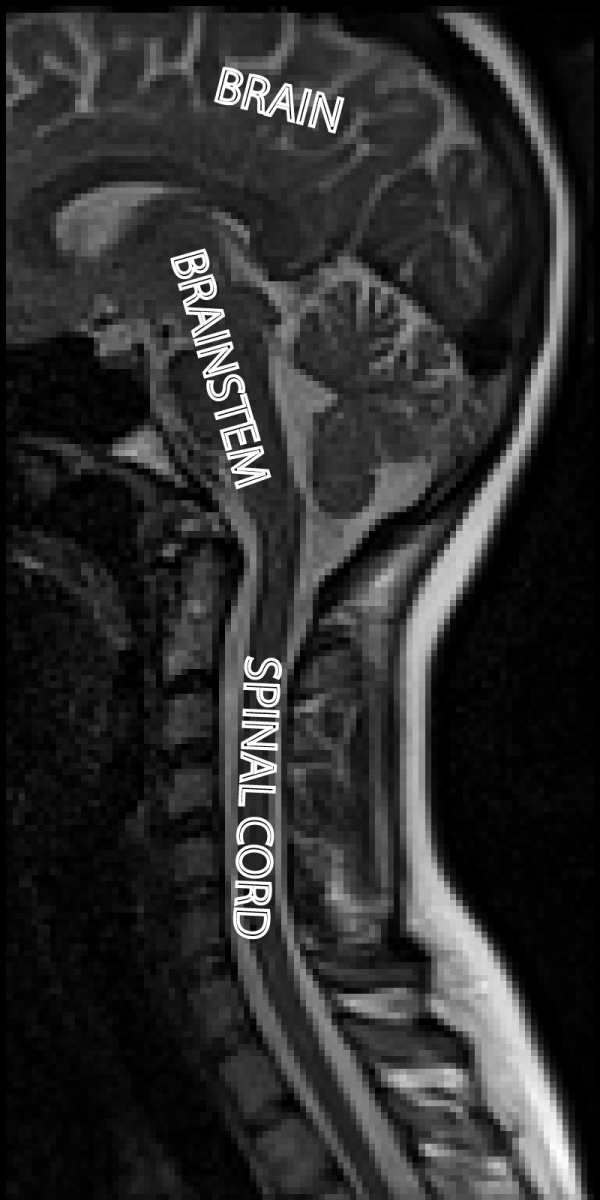
Our current basic understanding of pain is that receptors in our skin that respond to noxious stimuli send neural signals to our spinal cord, where they are processed and relayed up to our brainstem and then our brain. This ultimately produces the pain that we feel. These signals, however, can change over time. They can change based on having a brief stimulus or a sustained one, or having several brief stimuli in a short time. They can be altered by injury or inflammation. These signals are also regulated (turned up or down) by other signals coming down from the brain and brainstem. This feed-back changes our pain depending on our situation (such as being afraid, angry, in danger, relaxed, safe, etc.). Problems with the pain neural system that produce excessive or unexpected pain can occur at any of the levels of this pain processing system (the receptors, the nerves carrying the signal, the spinal cord, the brainstem, the brain, or a combination of many).
 FMRI has several important capabilities though. With it we can study neural processes in humans (albeit indirectly) and observe how pain processing works while people are awake, comfortable, and able to communicate with us throughout the study. However, these methods are still under development and always improving, so much of our focus is on using fMRI the most efficiently we can to study pain.
FMRI has several important capabilities though. With it we can study neural processes in humans (albeit indirectly) and observe how pain processing works while people are awake, comfortable, and able to communicate with us throughout the study. However, these methods are still under development and always improving, so much of our focus is on using fMRI the most efficiently we can to study pain.
The problem with pain research is that almost all of the fMRI studies since it was developed 30 years ago have been done in the brain. The brainstem and spinal cord are key components of the pain processing system, but early fMRI only allowed us to study the brain. Research in the Stroman Lab is quite unique, and for the past 20 years has focused on developing fMRI methods for the brainstem and spinal cord with a large degree of success. More than half of the research papers published on spinal cord fMRI have been from our lab. However, there is still more work to do in order to make fMRI really effective for pain research.
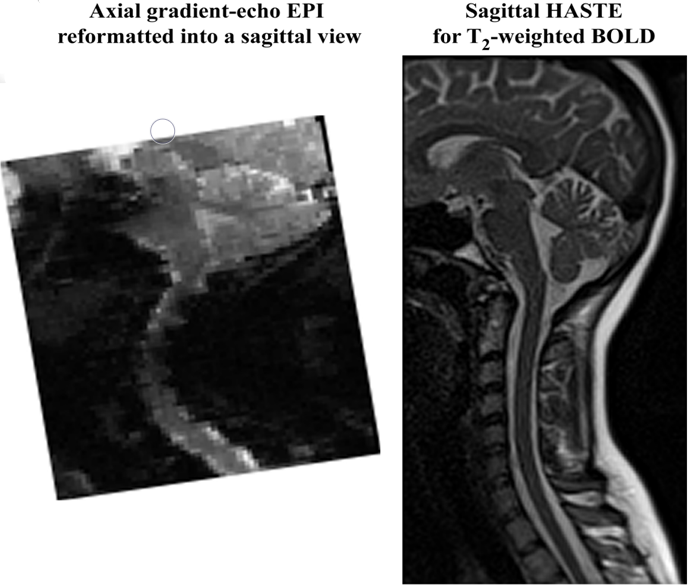 The methods to acquire data that are effective in the brain are not adequate in the brainstem and spinal cord. In order to adapt fMRI for studying pain, methods needed to be selected for imaging the brainstem and spinal cord, because these regions are more challenging to image than the brain. These methods have their advantages (such as being equally sensitive to BOLD changes but with less distortions in the spinal cord) and their disadvantages (such as being slower). It is more important to acquire good data at the cost of doing it slightly slower, than to acquire a lot of poor data really quickly.
The methods to acquire data that are effective in the brain are not adequate in the brainstem and spinal cord. In order to adapt fMRI for studying pain, methods needed to be selected for imaging the brainstem and spinal cord, because these regions are more challenging to image than the brain. These methods have their advantages (such as being equally sensitive to BOLD changes but with less distortions in the spinal cord) and their disadvantages (such as being slower). It is more important to acquire good data at the cost of doing it slightly slower, than to acquire a lot of poor data really quickly.
Figure(left): These two images show the lower part of the head, and the neck, in the same person. Imagine you are looking at the person from the side, and they are facing toward the left. The image on the left was acquired with the standard fMRI acquisition method (gradient-echo EPI). The image on the right was acquired with the HASTE method. Note that these images are of the same person, in the same scanner, on the same day. Your choice of methods can make a big difference to your quality of data. The image on the left is severely distorted, and the brainstem and spinal cord are not well-represented. These two imaging methods have approximately equal sensitivity for fMRI. The HASTE method is slower, but accurately represents the anatomy, which is essential for fMRI studies.
To do our studies, we also had to develop an MRI-compatible device that could apply a brief stimulus with a specific, controllable, temperature, at the exact timing that we needed. This stimulus is set to be hot enough to be painful, but not too hot as to cause injury. We developed the “MRI-compatible robotic contact heat thermal stimulator”, called RTS-2.
After acquiring our data, we need to analyze it to be able to interpret our results and draw conclusions from them. These analysis methods also need to be adapted for the brainstem and spinal cord regions as well. Custom-written analysis software has been developed by P. Stroman for about 25 years, in both MATLAB and python (programming languages). This process is still on-going as improvements continue to be made.
In addition, methods also need to be adapted for the complex process of experiencing pain. Our results showed that pain regulation is continuous – that is, it occurs all the time, even when we are not feeling pain – and it can be affected by our situation, mood, attention focus, etc. We hypothesized that this continuous component of regulation is of key importance for understanding pain, and how chronic pain conditions can develop. Our methods need to account for the fact that pain regulation is continuous (and doesn’t just occur right as someone is feeling pain).
One problem with our analysis approach though, is that it does not match conventional fMRI analysis methods. The most common fMRI analysis method is to predict the BOLD response, and to analyze the data to see where it occurs. The continuous component varies between people, and depends on emotional and cognitive factors, and, for now, is somewhat unpredictable (except for the consistent features we have observed).
We therefore turned to analysis methods that are “data-driven” and do not require a predicted model of the BOLD response.
Now, we are applying these methods to study how pain processing in fibromyalgia is different than in healthy people without fibromyalgia. We are also continuing to develop the fMRI methods that are well-matched to studying pain.
