Unraveling the mysteries of a brain disease
September 21, 2022
Share
Alzheimer’s Disease (AD) affects memory, thinking, and behaviour, and is the most common form of dementia, contributing to 60-70 per cent of cases worldwide. In Canada alone, over 500,000 people live with dementia – a number that is expected to be closer to a million by 2030. Raising awareness about AD and all forms of dementia is the main goal of World Alzheimer’s Month, a campaign led each September by Alzheimer’s Disease International.

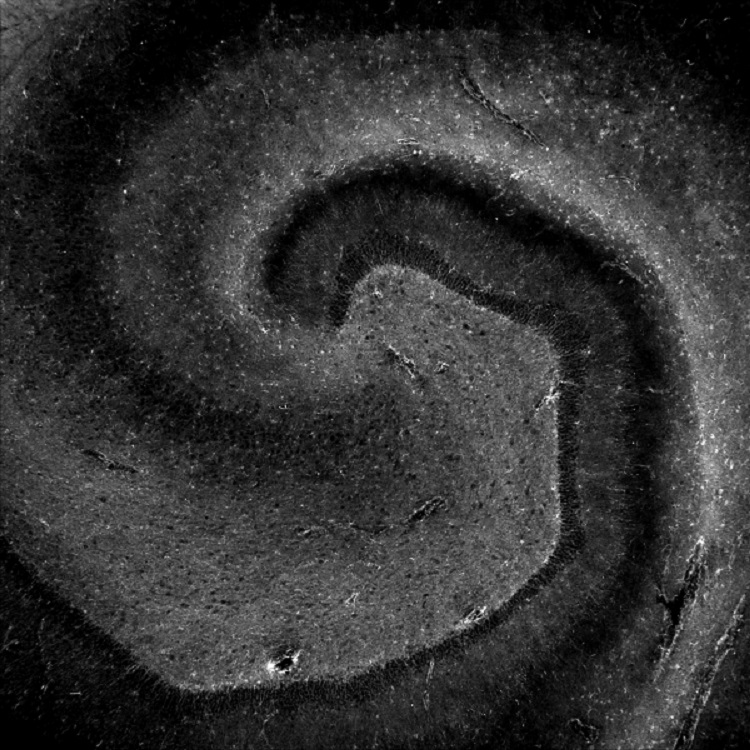
At Queen’s, Fernanda de Felice, associate professor in the departments of Biomedical and Molecular Sciences (DBMS) and Psychiatry and a member of the Centre for Neuroscience Studies (CNS), has dedicated over two decades of her research to understanding the molecular mechanisms of Alzheimer’s disease. Her team published a seminal study in 2019 on how hormones produced during physical activity can help protect the brain and slow Alzheimer’s progression.
De Felice recently spoke to the Gazette about the connections between the brain and metabolism, perspectives for future strategies to combat Alzheimer’s, and what AD and COVID-19 have in common.
Why did you decide to investigate the links between Alzheimer’s Disease and metabolism?
I started studying this specific area during my post-doc. At that time, we began to see some connections between AD and diabetes. Research showed that patients with diabetes had a higher risk of having AD. Other studies also suggested insulin signaling was altered in AD patients’ brains.
I was curious about the molecular mechanisms that connect these two diseases. We already knew how insulin resistance works in patients with diabetes, and we observed similar mechanisms in the brains with AD. From there, I moved on to study the effects of other hormones in the brain in the context of AD.
What did we learn about our brains and dementia by studying metabolism?
Today, it is widely known that what happens in our bodies can also influence our brains. We know that physical exercise, for example, benefits the brain. We know that our gut microbiota relates to mental health issues like depression, and so on.
While Alzheimer’s is a brain disease that presents later in life, it likely originates from health events and exposures earlier in one’s life. If we can understand how our metabolism impacts our brains, we can potentially develop strategies to prevent, or at least to delay, AD.
How can we stop Alzheimer’s?
An important topic in research is finding biomarkers for early AD diagnosis.
By the time a patient develops symptoms, there is already significant brain damage, and that is hard to reverse. In other words, it is difficult to treat AD, which is why it is crucial that we develop strategies to diagnose it early and delay its symptoms.
What we see in our findings is that a sustained healthy lifestyle, including physical activity and healthy eating, goes a long way. But AD is a multifactor disease, a combination of many aspects of our organism. That’s what makes it so challenging to treat and diagnose this form of dementia.
If Alzheimer’s and diabetes share the same molecular mechanisms, can we hypothesize that diabetes’ drugs can help us treat Alzheimer’s?
Currently, researchers are looking at administering these drugs to patients with mild cognitive impairment. While there have been some research studies in this area, we haven’t seen much improvement in patients with dementia treated with insulin. However, there are other possibilities.
In a study with Douglas Munoz (also a professor in DBMS and CNS), we obtained exciting results using diabetes drug liraglutide in pre-clinical models. A clinical trial launched in 2021 is investigating the effects of semaglutide in patients with early AD.
We do know that patients with obesity and diabetes who are treated for insulin resistance perform better in cognitive tests than the ones who are not treated. This signals that this kind of intervention might work if started in Alzheimer’s early stages, before there has been much brain damage.
Can you tell us more about your research on the impacts of COVID-19 on the brain? How does it relate to the field of brain-metabolism interactions?
Around 30 per cent of COVID-19 patients have some sort of neurological symptom, like concentration and memory problems, “brain fog,” and others. We did a study with samples of cerebrospinal fluid of COVID-19 patients, trying to understand what was happening – the molecular mechanisms of those neurological symptoms.
We could not find the virus, nor its proteins, in the samples. However, we found that some biomarkers of neurodegenerative pathologies – the same biomarkers we see in AD patients – were there.
We are now working on a longitudinal study with COVID-19 patients who did not have neurological symptoms. We want to know if they will have any alterations in the 18 months following infection. So far, we can say that some patients without any neurological symptoms in the acute phase of infection did have a cognitive decline after COVID-19.
I am interested in understanding what happens in their brains, and then comparing it to the brains of patients with AD.